Excess glucose in the bloodstream, known as hyperglycemia, can cause significant damage to cells and tissues throughout the human body, especially during prolonged periods of high blood sugar (hyperglycemia). Here's a breakdown of how it happens:
Glucose Overload and Oxidative Stress
When cells are overwhelmed with glucose, they start producing excess reactive oxygen species (ROS) — unstable molecules that damage DNA, proteins, and cell membranes. This process is known as oxidative stress.
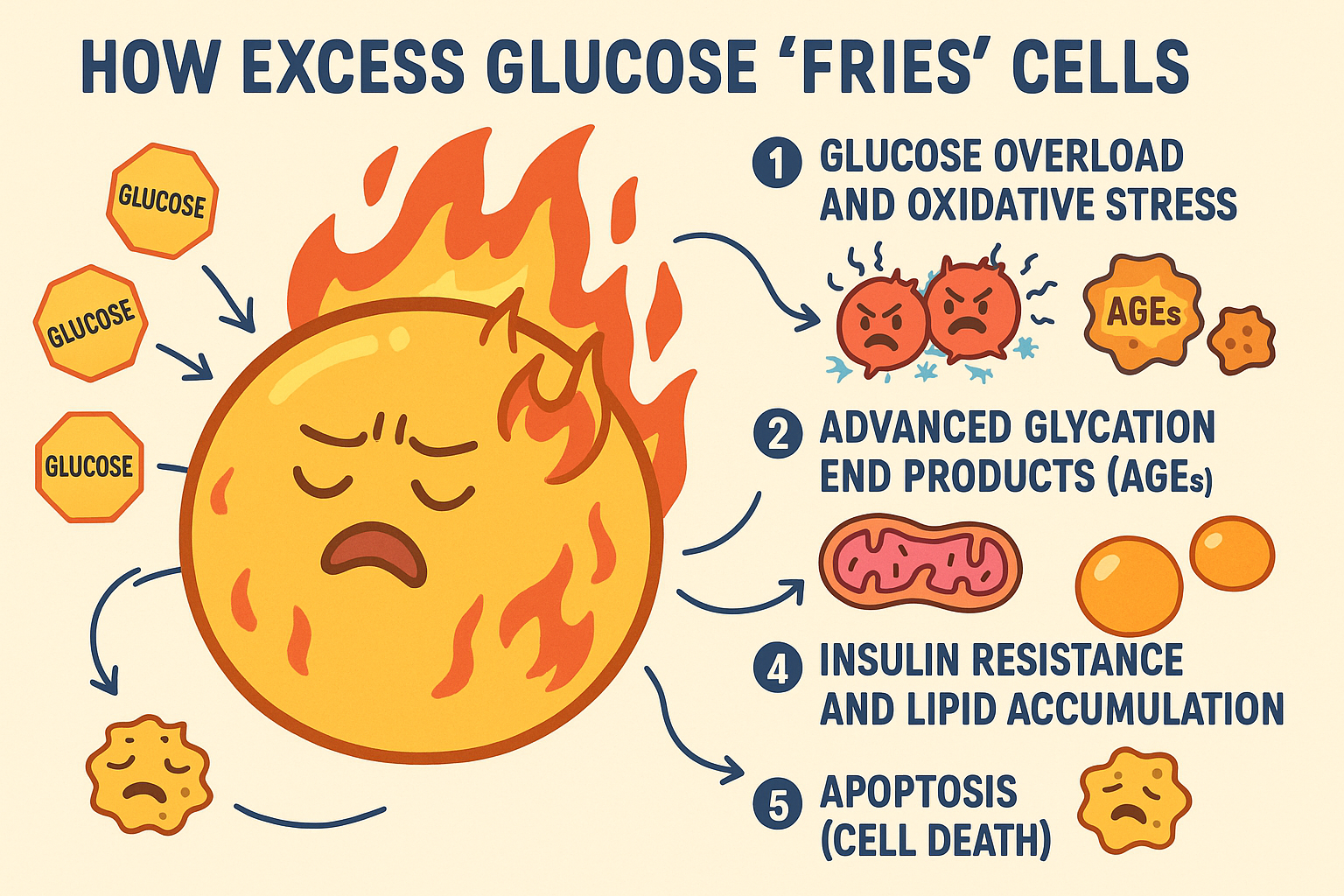
Advanced Glycation End Products (AGEs)
Excess glucose reacts with proteins and fats non-enzymatically, forming AGEs. These molecules:
- Disrupt protein structure and function
- Trigger inflammation
- Damage blood vessels and organs
This "glycation" is a major factor in the complications of diabetes.
Mitochondrial Overload
Cells (especially muscle and nerve cells) convert glucose into ATP using mitochondria. Too much glucose floods the mitochondria, causing them to:
- Leak electrons
- Produce excess ROS
- Dysfunction or die (a bit like overheating a machine)
Insulin Resistance and Lipid Accumulation
Chronically high glucose leads to insulin resistance, especially in fat and liver cells. Glucose can't enter cells efficiently, so blood sugar stays high, and the body turns more sugar into fat:
Fat builds up in non-fat tissues (liver, muscle).
This causes lipotoxicity, which contributes to cellular inflammation and death.
Apoptosis (Cell Death)
If the stress continues, cells may trigger their self-destruct mechanism (apoptosis) as a last resort to prevent further damage to surrounding tissue.
Analogy: Why "Fried"?
Just like food burns when exposed to excess heat/oil, cells get "fried" when exposed to too much fuel (glucose).
The "burning" isn't literal, but rather refers to oxidative and metabolic damage.